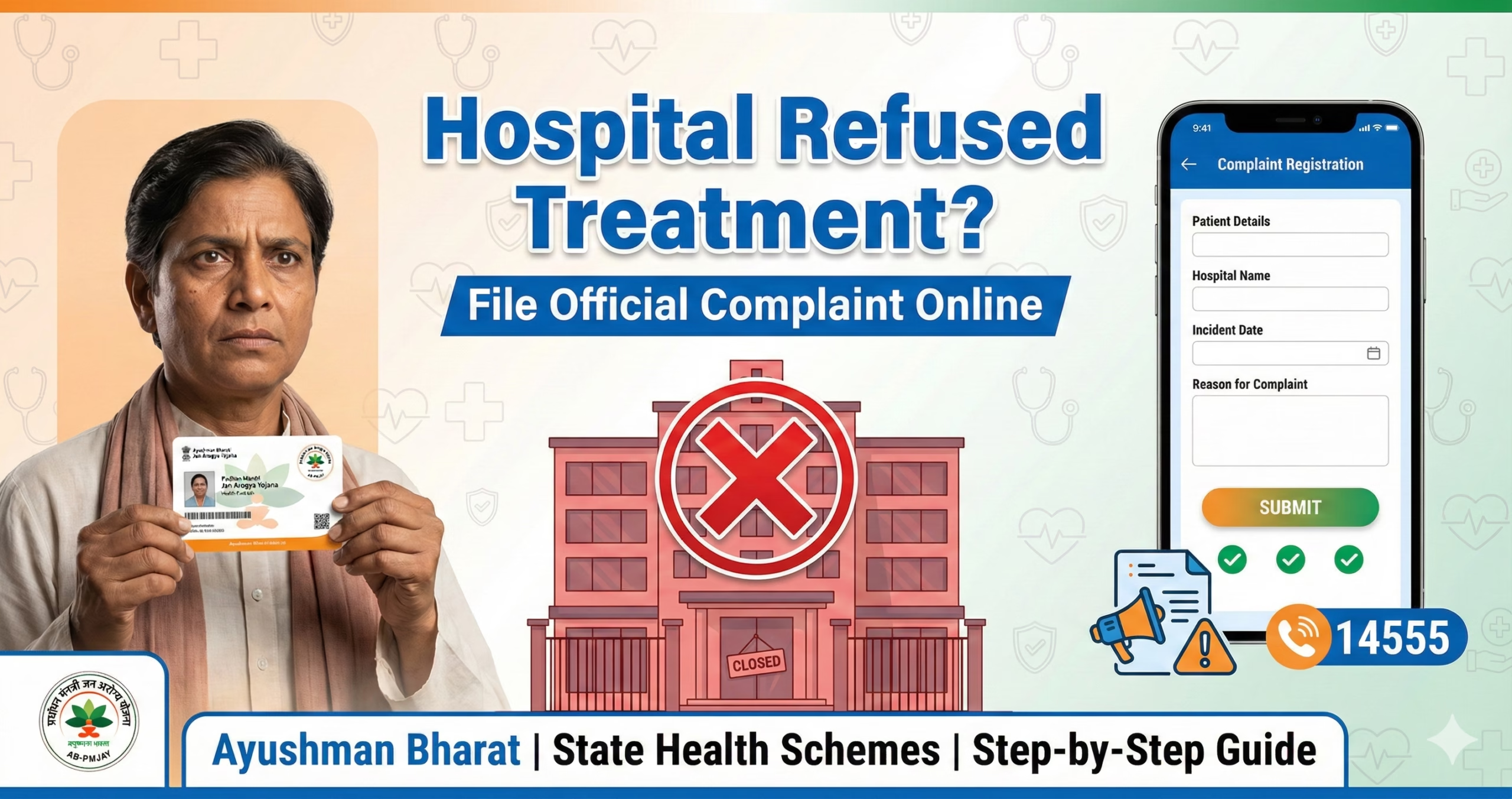
Who Needs This Service?
This complaint mechanism is for Indian citizens who have been denied treatment at empanelled hospitals under government health insurance schemes like Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY), state health schemes, CGHS, ECHS, or other government-sponsored health programs. If you possess a valid health card under any government scheme and a hospital refuses to provide cashless treatment or denies admission, you can file an official complaint.
Required Documents
Before filing a complaint, keep these documents ready:
- Valid Ayushman Bharat card/State health scheme card with Beneficiary ID
- Aadhaar card of the patient
- Mobile number registered with Aadhaar for OTP verification
- Hospital name, address, and UHID (if provided)
- Date and time of denial of treatment
- Doctor’s name or hospital staff details who refused treatment
- Any written communication or prescription from the hospital
- Medical reports or emergency case papers (if available)
- Photographs or screenshots of denial (if any)
- Witness details (if someone accompanied the patient)
Online Complaint Process for Ayushman Bharat (AB PM-JAY)
Step 1: Visit the Official Grievance Portal
Go to the official National Health Authority grievance portal: https://bis.pmjay.gov.in/BIS/beneLogin or the main portal https://pmjay.gov.in
On the homepage, look for “Grievance” or “Register Complaint” section. The beneficiary login portal allows you to file complaints directly.
Step 2: Register/Login as Beneficiary
- Click on “Beneficiary Login” on the portal
- Enter your Ayushman Bharat Beneficiary ID (11-digit number on your card)
- Enter registered mobile number
- Click “Generate OTP”
- Enter the 6-digit OTP received on your mobile
- Click “Login”
If you don’t have your Beneficiary ID, you can search using:
- Aadhaar number
- Ration card number
- Mobile number registered during enrollment
Step 3: Navigate to Complaint/Grievance Section
After successful login:
- Look for “Register Grievance” or “File Complaint” option in the dashboard
- Click on “New Complaint” or “Lodge Grievance”
- Select complaint category: “Denial of Treatment” or “Hospital Refused Cashless Treatment”
Step 4: Fill Complaint Details
You will see a complaint form with following fields:
- State: Select your state from dropdown
- District: Select your district
- Hospital Name: Select from empanelled hospital list or type hospital name
- Hospital Code/ID: Auto-populated or select from list
- Nature of Complaint: Select “Denial of Treatment” or “Refusal of Cashless Service”
- Date of Incident: Enter the date when treatment was refused
- Detailed Description: Write complete details in 500-1000 characters:
- What treatment was needed
- Why hospital refused (reason given by hospital)
- Staff/doctor name who denied
- Emergency or planned treatment
- Any amount demanded by hospital
Step 5: Upload Supporting Documents
- Click “Upload Documents” button
- Attach scanned copies of: Ayushman card, Aadhaar, hospital denial letter, medical reports
- Maximum file size: Usually 2MB per document
- Accepted formats: PDF, JPG, JPEG, PNG
- You can upload up to 5 documents
Step 6: Submit Complaint
- Review all entered information carefully
- Check mobile number for updates
- Click “Submit Complaint” button
- A complaint registration number will be generated (format: PMJAY/GR/XXXXXX/2026)
- Save this number for tracking
- You will receive SMS confirmation on registered mobile
Step 7: Alternative Toll-Free Number Complaint
If you cannot access internet, call the Ayushman Bharat toll-free helpline:
14555 or 1800-111-565
- Call between 9 AM to 6 PM on working days
- Select language preference
- Choose option for “Complaint Registration”
- Provide your Ayushman Bharat ID
- Explain the denial of treatment issue
- Operator will register complaint and provide complaint number
- You will receive SMS with complaint reference number
State-Specific Health Scheme Complaint Process
For State Health Schemes
Different states have their own complaint mechanisms:
1. Delhi (DGEHS – Delhi Government Employees Health Scheme)
- Portal: https://edistrict.delhigovt.nic.in
- Navigate to Health Services → Grievance
- Or call: 1800-110-058
2. Maharashtra (Mahatma Jyotiba Phule Jan Arogya Yojana)
- Portal: https://www.jeevandayee.gov.in
- Click on “Register Complaint”
- Or call: 1800-102-2708
3. Tamil Nadu (Chief Minister’s Comprehensive Health Insurance Scheme)
- Portal: https://www.cmchistn.com
- Grievance section
- Or call: 044-2530-3701
4. Karnataka (Suvarna Arogya Suraksha)
- Portal: https://ahkarhfw.karnataka.gov.in
- Or call: 104 (State Health Helpline)
5. West Bengal (Swasthya Sathi)
- Portal: https://swasthyasathi.gov.in
- Click “Grievance Redressal”
- Or call: 1800-313-4321
6. Rajasthan (Bhamashah Swasthya Bima Yojana)
- Portal: https://health.rajasthan.gov.in
- Or call: 18001806127
For other states, visit your State Health Department website and look for health insurance/scheme grievance sections.
Offline Complaint Process
District Health Office Complaint
If online access is not available:
- Visit District Health Office: Go to the Chief Medical Officer (CMO) or District Health Office in your district
- Submit Written Complaint: Prepare a written complaint in this format:
- To: The Chief Medical Officer/District Nodal Officer
- Subject: Complaint against [Hospital Name] for denial of treatment under [Scheme Name]
- Body: Include all details – your beneficiary ID, hospital name, date of denial, reason given, emergency nature
- Attach photocopies of all documents
- Obtain Acknowledgment: Insist on a complaint receipt with date and registration number
- Contact Details: Find your district health office contact from https://nhm.gov.in or state health department website
Complaint to National Health Authority (NHA)
For serious cases, send written complaint to:
National Health Authority 9th Floor, Tower-l, Jeevan Bharati Building Connaught Place, New Delhi – 110001 Email: grievance@nha.gov.in
Include all documents and mention your previous complaint number if any.
Insurance Company Complaint (TPA)
Since AB PM-JAY works through Third Party Administrators:
- Contact the TPA managing the hospital
- TPA details are available on hospital board or PMJAY website
- Email the TPA with complaint details
- Common TPAs: ICICI Lombard, New India Assurance, Star Health, etc.
How to Track Your Complaint Status
Online Status Check
- Visit Grievance Portal: https://bis.pmjay.gov.in/BIS/beneLogin
- Login: Use your Beneficiary ID and mobile OTP
- Check Status:
- Click on “Track Complaint” or “My Grievances”
- Enter complaint registration number
- View current status: Registered/Under Review/Resolved/Closed
- Status Updates:
- You will receive SMS updates at each stage
- Email updates if email ID was provided
- Typical resolution time: 15-30 days
Through Helpline
- Call 14555 or 1800-111-565
- Provide complaint registration number
- Operator will inform current status
District Office Follow-Up
- Visit district health office after 7 days if no response
- Carry complaint acknowledgment receipt
- Meet the concerned officer for status update
Common Problems and Solutions
1. Hospital Says “Scheme Card Not Valid” or “Not Accepted Here”
Solution:
- Verify hospital is empanelled: Check on https://hospitals.pmjay.gov.in
- Search your hospital by name/state/district
- If hospital is empanelled but still refusing, immediately call 14555 and file complaint
- Request written refusal from hospital for evidence
- In genuine emergencies, hospital CANNOT refuse treatment under AB PM-JAY rules
2. Complaint Registration Number Not Generated
Solution:
- Check internet connection and retry
- Clear browser cache and cookies
- Try different browser (Chrome, Firefox)
- Use mobile app if available
- If technical error persists, call helpline 14555 to register complaint verbally
- Take screenshot of error message for reference
3. OTP Not Received for Login
Solution:
- Verify mobile number is same as registered during enrollment
- Check if mobile number is in DND (Do Not Disturb) – disable it temporarily
- Wait 2-3 minutes before requesting new OTP
- Check spam/message filters
- If issue persists, use “Login with Aadhaar OTP” option
- Contact helpline to update mobile number if changed
4. Hospital Not Listed in Dropdown Menu
Solution:
- Type hospital name manually in search box
- Select “Other” option and type complete hospital name and address
- Hospital empanelment can be verified at https://hospitals.pmjay.gov.in/empanelledhospitals
- If hospital claims empanelment but not listed, mention this in complaint description
- Contact State Health Agency for verification
5. No Response Even After 30 Days
Solution:
- Escalate to National Health Authority email: grievance@nha.gov.in
- File RTI application asking for complaint status and action taken
- Approach District Collector’s office with written complaint
- Contact State Health Minister’s office (details on state government website)
- Tweet to @AyushmanNHA or @PMJAYGov with complaint number (public complaints get faster response)
- As last resort, approach Consumer Court for medical negligence/denial of service
Immediate Action for Medical Emergencies
If treatment is denied in emergency situations:
- Call 108/102 Ambulance: Request transfer to another empanelled hospital
- Call 14555 Immediately: Report denial while at hospital premises
- Record Denial: If possible, audio/video record hospital staff refusing treatment (legal in emergency situations)
- Inform Local Authority: Call local police (100) if patient’s life is at risk due to denial
- Approach Another Hospital: Don’t waste time arguing; patient’s life is priority
- File Complaint Later: After emergency is handled, file detailed complaint
Under AB PM-JAY and most state schemes, empanelled hospitals cannot refuse treatment in emergencies. This is a violation of scheme guidelines and Medical Council of India regulations.
Official Helpline Numbers and Contacts
Ayushman Bharat PM-JAY
- Toll-Free: 14555 (All days, 9 AM – 6 PM)
- Alternate: 1800-111-565
- Email: grievance@nha.gov.in
- Website: https://pmjay.gov.in
- Twitter: @AyushmanNHA
CGHS (Central Government Health Scheme)
- Helpline: 1800-180-1515
- Email: cghs@gov.in
- Website: https://cghs.nic.in
ECHS (Ex-Servicemen Contributory Health Scheme)
- Helpline: 1800-102-1095
- Email: complaintcell-echs@gov.in
- Website: https://echs.gov.in
State Health Department Contacts
- Find your state’s health department contact: https://nhm.gov.in/index1.php?lang=1&level=1&sublinkid=150&lid=49
Insurance Regulatory and Development Authority of India (IRDAI)
For complaints against TPAs/Insurance companies:
- Website: https://igms.irda.gov.in
- Email: complaints@irdai.gov.in
- Toll-Free: 155255
What Happens After Complaint Registration
- Acknowledgment: You receive complaint number within 24 hours
- Investigation: District officials/TPA investigates within 7 days
- Notice to Hospital: Hospital asked to provide explanation
- Action: Based on findings:
- Hospital directed to provide treatment
- Hospital may be de-empanelled for serious violations
- Financial penalty on hospital
- Your treatment arranged at another hospital
- Closure: Complaint closed after resolution; you receive closure notification
Your Rights Under Government Health Schemes
- Right to cashless treatment at any empanelled hospital
- Right to emergency treatment without any advance payment
- Right to choose hospital from empanelled list
- Right to quality treatment as per package rates
- Right to file complaint without fear of denial
- Right to receive treatment summary and discharge card
Remember: Government health schemes are your legal right. No hospital can demand money for covered treatments or refuse admission if empanelled under the scheme.
This information is from official sources including National Health Authority (https://pmjay.gov.in), Ministry of Health and Family Welfare portals, and state health department websites as of February 2026. Always verify on the official portal for the latest updates and state-specific procedures. Scheme guidelines and portal interfaces may be updated periodically by the government.